A lack of rapid cardiopulmonary resuscitation (CPR) or rapid defibrillation causes more than 350,000 U.S. deaths annually. Emergency medical services (EMS) responders and bystander CPR can double a person’s chances of survival from an out-of-hospital cardiac arrest (OHCA).
A new study reported in the Journal of the American College of Cardiology sought to evaluate the potential impact of the pandemic on OHCA. Does fear of infection inhibit bystanders from offering assistance? Do new screening procedures for 911 calls affect the time it takes for EMS responders to arrive?
The researchers hypothesized that with COVID-19, “community response to OHCA and EMS processes for responding to OHCA would be altered, with negative effects on survival outcomes.”
Researchers looked at data from two U.S. counties, Oregon’s Multnomah (where Portland is located) and Ventura County, California, gathered between March 1 and May 31 for 2019 and 2020. These locations were selected because they had high COVID-19 infection rates.
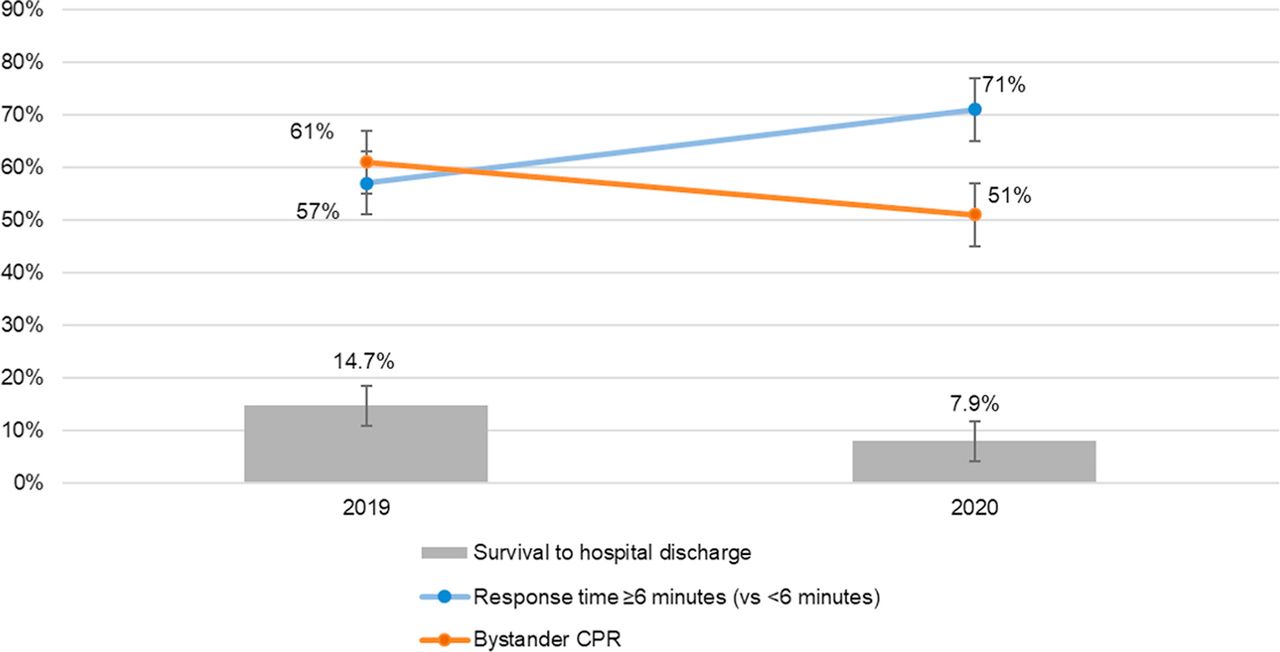
There were 231 OHCA incidents in 2019 and 278 in 2020. In 61% of the 2019 incidents, bystanders provided CPR to a person having a cardiac arrest. In 2020, the percentage dropped to 51%. Similarly, bystanders equipped with automated external defibrillators provided assistance in 5% of 2019 incidents compared to just 1% in 2020.
The following chart graphs the difference between bystander CPR (orange line), response time for emergency medical services (blue line) and survival rate. According to the study, incidence rates did not change significantly and coronavirus infection rates were low.
The study’s authors concluded that less bystander CPR, longer response times from emergency services and lower survival rates “highlight the pandemic’s indirect negative impact on OHCA even in communities with relatively low incidence of COVID-19.”
Whether patients delayed calling 911 was not part of this study, but the researchers noted another study that reported a “steep” nationwide decline in hospital-treated acute coronary syndrome during the early pandemic period. That decline indicates that fewer people were seeking care for cardiac symptoms. Why?
According to studies cited by Consumer Reports, about half of adults who lost their jobs or income due to the pandemic avoided health care facilities, either due to cost or concern about getting infected. A Centers for Disease Control and Prevention (CDC) study found that emergency room visits were 42% lower year over year in March and April this year.
CDC data also showed that deaths related to heart disease and other non-COVID-19 causes were higher than normal. That may have been due to undiagnosed coronavirus infections or to people not getting the medical care they needed.
Higher death rates due to increased response times were reported in a study last year that determined health care facilities recovering from a data breach essentially wiped out improvements in treating heart attack victims due to increased response times.
Take Charge of Your Retirement: Find the Right Financial Advisor For You in Minutes (Sponsor)
Retirement planning doesn’t have to feel overwhelming. The key is finding professional guidance—and we’ve made it easier than ever for you to connect with the right financial advisor for your unique needs.
Here’s how it works:
1️ Answer a Few Simple Questions
Tell us a bit about your goals and preferences—it only takes a few minutes!
2️ Get Your Top Advisor Matches
This tool matches you with qualified advisors who specialize in helping people like you achieve financial success.
3️ Choose Your Best Fit
Review their profiles, schedule an introductory meeting, and select the advisor who feels right for you.
Why wait? Start building the retirement you’ve always dreamed of. Click here to get started today!
Thank you for reading! Have some feedback for us?
Contact the 24/7 Wall St. editorial team.