Special Report
The Least Healthy City in Every State

Published:
Last Updated:

Life expectancy is one of the most telling and often cited measures of the health of a given population — and in the United States, life expectancy is falling at a historic rate. After declining for three consecutive years, life expectancy at birth stands at 78.6 years. It is too early to tell what impact on life expectancy the COVID-19 pandemic will have, but according to one estimate published at Prevent Epidemics website, the pandemic could lower life expectancy by at least five years in New York City, one the earlier epicenters of the outbreak in the U.S.
In a 2017 report, the Centers for Disease Control and Prevention identified several factors contributing to the decline in life expectancy. These include climbing rates of several diseases and conditions such as stroke, diabetes, and chronic liver disease, as well as unintentional injuries, which notably include drug overdoses. These conditions are often connected to unhealthy lifestyles — and in some parts of the country, both unhealthy behaviors and poor health outcomes are more common than in others.
24/7 Tempo created a weighted index of 35 measures of health outcomes and health factors, including behaviors and access to care, and ranked the 381 U.S. metropolitan areas based on the index to identify the least healthy metropolitan area in every state. Index measures include smoking rates, adult obesity rates, premature death rates, shares of adults who exercise regularly, health insurance coverage, and unemployment rate.
Making the list as the least healthy city in a state does not necessarily mean a particular metro area is unhealthy compared to the United States as a whole. Some states have relatively healthy populations and average life expectancies that exceed the national average by several years — these are the states where people live the longest.
The cities on this list tend to share certain socioeconomic characteristics. For example, in 43 metro areas on this list, the median annual household income is lower than the median across the state as a whole. This is likely no coincidence, as lower-income Americans tend to have less access to health care as well as to healthy options related to diet and lifestyle, and therefore they often report worse health outcomes than wealthier Americans.
A high uninsured rate is also common among the counties on this list. Americans without health insurance are less likely to make regular doctor visits, receive treatments, and receive preventative care. Many of the 50 metro areas on this list have the highest share of adults without health insurance in their respective state.
Click here for the least healthy city in every state
Click here for our detailed methodology

Alabama: Mobile
> Adult obesity rate: 36.3% (state: 35.5%)
> Adult smoking rate: 19.4% (state: 20.9%)
> Pct. of adults who don’t exercise: 30.6% (state: 29.8%)
> Residents with no health insurance: 11.7% (state: 11.0%)
> Median household income: $49,561 (state: $51,734)
Unhealthy lifestyles are relatively common in Mobile, Alabama. Adults in the metro area are more likely to be obese than adults across the state as a whole. They are also less likely to exercise. About 30.6% of adults in the metro area have sedentary lifestyles, slightly more than the state average of 29.8% of adults who do not exercise and well above the national average of 23.0%.
Unhealthy habits may be taking a toll. The age-adjusted premature death rate of 496 deaths before age 75 for every 100,000 people annually is well above the premature death rate statewide of 475 per 100,000 and is the 22nd highest rate of any metro area in the U.S.
[in-text-ad]
Alaska: Anchorage
> Adult obesity rate: 32.5% (state: 32.5%)
> Adult smoking rate: 15.7% (state: 21.0%)
> Pct. of adults who don’t exercise: 18.7% (state: 20.0%)
> Residents with no health insurance: 13.3% (state: 14.8%)
> Median household income: $80,676 (state: $75,463)
Of the two metro areas in Alaska — Anchorage and Fairbanks — Anchorage ranks as the least healthy. Adults in Anchorage are less likely to exercise regularly and slightly more likely to be obese than those living in Fairbanks.
Those who are unemployed are more likely to have certain unhealthy behaviors and report worse health outcomes than those who are employed. In Anchorage, the annual unemployment rate stands at 5.5%, slightly higher than the 5.4% rate in Fairbanks.

Arizona: Lake Havasu City-Kingman
> Adult obesity rate: 31.8% (state: 27.5%)
> Adult smoking rate: 19.4% (state: 15.6%)
> Pct. of adults who don’t exercise: 32.2% (state: 21.8%)
> Residents with no health insurance: 13.4% (state: 12.1%)
> Median household income: $50,179 (state: $62,055)
Lake Havasu City has the highest premature death rate of any of the seven metro areas in Arizona. There are 503 deaths before age 75 annually for every 100,000 people in the metro area, compared to a statewide rate of 332 per 100,000.
Such negative health outcomes are likely partially attributable to unhealthy lifestyles in the metro area. For example, 19.4% of adults in Lake Havasu City smoke, compared to 15.6% of adults statewide. Additionally, 31.8% of area adults are obese, compared to 27.5% of adults across the state. Obesity is a risk factor for a number of potentially fatal diseases and conditions, including heart disease, diabetes, and certain cancers.

Arkansas: Pine Bluff
> Adult obesity rate: 39.3% (state: 34.2%)
> Adult smoking rate: 21.3% (state: 22.3%)
> Pct. of adults who don’t exercise: 34.9% (state: 31.6%)
> Residents with no health insurance: 7.6% (state: 9.3%)
> Median household income: $41,541 (state: $48,952)
Pine Bluff is the least healthy metro area in Arkansas and one of the least healthy nationwide. About 39.3% of adults are obese, one of the largest shares of all 381 metro areas in the country. The state’s adult obesity rate is 34.2%, and the national rate is 29.0%. Obesity is a risk factor for a number of potentially deadly diseases and conditions, including diabetes, heart disease, and certain cancers. Premature death is far more common in Pine Bluff than it is across the state as a whole. For every 100,000 people in the metro area, there are 563 deaths before age 75 annually, compared to a rate of 460 deaths per 100,000 people across Arkansas.
Lower-income Americans have less access to quality health care options than those with higher incomes, and they are less able to afford living a healthy lifestyle. In Pine Bluff, the typical household earns just $41,541 a year, one of the lowest median household incomes of all U.S. metro areas and lower than the state median of $48,952 and the national median of $65,712.
[in-text-ad-2]

California: Bakersfield
> Adult obesity rate: 32.3% (state: 23.6%)
> Adult smoking rate: 15.3% (state: 11.3%)
> Pct. of adults who don’t exercise: 22.4% (state: 17.6%)
> Residents with no health insurance: 8.6% (state: 8.2%)
> Median household income: $53,067 (state: $80,440)
Of the 26 metro areas in California, Bakersfield is the least healthy. Smoking is the leading cause of preventable death in the United States, and in Bakersfield, 15.3% of adults are smokers, the largest share of any metro area in the state and higher than the statewide smoking rate of 11.3%. Bakersfield residents are also far less likely to exercise than the typical Californian. Just 77.6% of metro area adults engage in some leisure-time physical activity, compared to 82.4% of adults across the state.
The prevalence of sedentary lifestyles in Bakersfield may be due in part to a lack of exercise opportunities. About 75.9% of metro area residents have access to places for exercise like parks or recreation centers, compared to over 93.1% of all Californians.

Colorado: Pueblo
> Adult obesity rate: 29.4% (state: 21.8%)
> Adult smoking rate: 16.4% (state: 14.6%)
> Pct. of adults who don’t exercise: 22.1% (state: 15.5%)
> Residents with no health insurance: 8.4% (state: 8.7%)
> Median household income: $51,276 (state: $77,127)
Pueblo is the only metro area in Colorado where adults report an average of more than four days of poor mental health in a month and more than four physically unhealthy days per month. Additionally, 22.5% of adults in the metro area report being in fair or poor health, by far the largest share in the state and one of the largest shares of any U.S. metro area. For context, 17.0% of American adults and 14.5% of adults in Colorado report being in fair or poor health.
Low-income Americans tend to have less access to health care options than those with higher incomes and are less able to afford leading a healthy lifestyle. In Pueblo, the typical household earns just $51,276 a year, significantly less than the median household income in Colorado of over $77,127.
[in-text-ad]

Connecticut: New Haven-Milford
> Adult obesity rate: 28.1% (state: 25.8%)
> Adult smoking rate: 12.8% (state: 12.7%)
> Pct. of adults who don’t exercise: 21.7% (state: 20.4%)
> Residents with no health insurance: 5.7% (state: 6.3%)
> Median household income: $69,751 (state: $78,833)
Adults in New Haven are more likely to report being in poor mental and physical health than those in any of the three other metro areas in Connecticut. Regular exercise can improve overall well-being, and adults in New Haven are less likely to be physically active than the average adult in the state.
Smoking is the leading cause of preventable death in the United States, and New Haven’s smoking rate of 12.8% is the highest of any metro area in the state. It is, however, still lower than the 17.0% national smoking rate.

Delaware: Dover
> Adult obesity rate: 35.4% (state: 30.9%)
> Adult smoking rate: 16.8% (state: 17.0%)
> Pct. of adults who don’t exercise: 31.2% (state: 27.7%)
> Residents with no health insurance: 6.4% (state: 6.1%)
> Median household income: $58,001 (state: $70,176)
Dover is the only metro area in Delaware and ranks as the least healthy city by default. By several important measures, the capital city is indeed less healthy than the state as a whole. For example, only 68.8% of metro area adults exercise regularly, compared to 72.3% of adults across the state. Regular physical activity can help in maintaining a healthy weight, and in Dover, 35.4% of adults are obese, a larger share than the 30.9% share of adults across the state.

Florida: Sebring
> Adult obesity rate: 30.5% (state: 26.6%)
> Adult smoking rate: 18.7% (state: 16.1%)
> Pct. of adults who don’t exercise: 33.3% (state: 25.9%)
> Residents with no health insurance: 18.5% (state: 16.0%)
> Median household income: $48,698 (state: $59,227)
The Sebring metro area ranks as the least healthy metro area in Florida and one of the least healthy nationwide. Just 66.7% of adults in Sebring exercise regularly, compared to 74.1% of adults statewide and 77.0% nationwide. Physical inactivity can increase the risk of obesity, and in Sebring 30.5% of adults are obese, more than the statewide obesity rate of 26.6% and the nationwide rate of 29.0%.
Obesity is a risk factor for many leading causes of premature death. In Sebring, 440 in every 100,000 residents die before the age of 75, far more than the statewide premature death rate of 339 per 100,000.
[in-text-ad-2]

Georgia: Albany
> Adult obesity rate: 40.9% (state: 32.0%)
> Adult smoking rate: 19.9% (state: 17.5%)
> Pct. of adults who don’t exercise: 29.9% (state: 27.5%)
> Residents with no health insurance: 14.8% (state: 15.5%)
> Median household income: $40,625 (state: $61,980)
Smoking is the leading cause of preventable death in the United States, and in Albany, Georgia, 19.9% of adults are smokers, the largest share of any of the state’s 14 metro areas. Unhealthy habits like smoking likely contribute to Albany’s higher than average premature death rate. There are 500 deaths before age 75 for every 100,000 Albany residents annually, well above the state rate of 381 premature deaths per 100,000.
Lower-income Americans have less access to quality health care than those with higher incomes, and they often report worse health outcomes as a result. In Albany, the typical household earns just $40,625 a year, well below the median household income of $61,980 across the state.

Hawaii: Kahului-Wailuku-Lahaina
> Adult obesity rate: 24.0% (state: 23.7%)
> Adult smoking rate: 12.3% (state: 12.8%)
> Pct. of adults who don’t exercise: 20.0% (state: 20.5%)
> Residents with no health insurance: 5.4% (state: 4.6%)
> Median household income: $80,754 (state: $83,102)
Of the two metro areas in Hawaii — Kahului-Wailuku-Lahaina and Honolulu — Kahului-Wailuku-Lahaina ranks as the least healthy. Residents of the Kahului metro area are slightly more likely to smoke and be obese than those living in Honolulu.
Still, compared to the rest of the state, the city is relatively healthy by some measures of self-reported health status. For example, only 12.9% of adults in the metro area report to be in fair or poor health, below the 14.2% share across the state.
[in-text-ad]
Idaho: Pocatello
> Adult obesity rate: 32.0% (state: 29.3%)
> Adult smoking rate: 14.4% (state: 14.3%)
> Pct. of adults who don’t exercise: 20.8% (state: 20.8%)
> Residents with no health insurance: 10.7% (state: 11.8%)
> Median household income: $51,612 (state: $60,999)
Adults in Pocatello are more likely to be obese than those across Idaho as a whole. The metro area’s adult smoking rate of 14.4% is the second highest of any metro area in the state. Both smoking and obesity are risk factors for a number of potentially deadly diseases and conditions, and in Pocatello, the premature death rate of 394 deaths before age 75 per 100,000 people is well above the state rate of 308 premature deaths per 100,000 people.
Self-reported health outcomes are also poor in Pocatello. Of the five metro areas in the state, Pocatello is the only one where adults report an average of more than four physically unhealthy days per month.

Illinois: Danville
> Adult obesity rate: 40.9% (state: 29.7%)
> Adult smoking rate: 17.7% (state: 15.5%)
> Pct. of adults who don’t exercise: 31.5% (state: 22.3%)
> Residents with no health insurance: 6.5% (state: 7.9%)
> Median household income: $43,111 (state: $69,187)
Danville is the least healthy metro area in Illinois and among the least healthy in the entire country. Some 17.7% of metro area adults smoke, compared to 15.5% of adults across the state and 17.0% of adults nationwide. Smoking is the leading cause of preventable death in the United States, and in Danville, the premature death rate of 489 deaths before age 75 annually for every 100,000 people is significantly higher than the state rate of 329 per 100,000.
Living in poverty can greatly reduce a person’s ability to access health care and make healthy lifestyle choices, and as a result, poorer Americans often report worse health outcomes. In Danville, the median household income is among the lowest of all 381 metro areas in the U.S. at $43,111. Statewide, the median annual household income is $69,187.
Indiana: Muncie
> Adult obesity rate: 34.1% (state: 33.4%)
> Adult smoking rate: 21.0% (state: 21.8%)
> Pct. of adults who don’t exercise: 27.9% (state: 26.7%)
> Residents with no health insurance: 9.0% (state: 9.6%)
> Median household income: $45,065 (state: $57,603)
Muncie has the second highest premature death rate of any of the 12 metro areas in Indiana. For every 100,000 Muncie residents, there are 506 deaths before age 75 annually, compared to the statewide premature death rate of 401 per 100,000. The metro area’s adult obesity rate of 34.1% is slightly higher than the state obesity rate of 33.4%.
A fifth of adults in the Muncie area report being in poor or fair health, more than any other metro area in the state. Muncie’s adult residents report more physically unhealthy days than the rest of Indiana’s residents, or about 4.5 days a month, compared to a statewide average of 4.2 and nationwide average of 3.8 physically unhealthy days a month.
[in-text-ad-2]

Iowa: Davenport-Moline-Rock Island
> Adult obesity rate: 33.8% (state: 33.2%)
> Adult smoking rate: 16.5% (state: 17.1%)
> Pct. of adults who don’t exercise: 23.8% (state: 23.7%)
> Residents with no health insurance: 5.8% (state: 5.5%)
> Median household income: $62,001 (state: $61,691)
Though Davenport ranks as the least healthy metro area in Iowa, area adults still tend to be healthier than the typical American by several health measures. For example, 15.4% of adults in the metro area report being in fair or poor health. While this is a larger share than the 14.5% of adults across the state reporting similarly low health status, it is lower than the nationwide figure of 17.0% of adults. Additionally, Davenport’s 16.5% smoking rate is lower than both the comparable state and national rates.

Kansas: Wichita
> Adult obesity rate: 34.0% (state: 33.2%)
> Adult smoking rate: 16.7% (state: 17.4%)
> Pct. of adults who don’t exercise: 26.0% (state: 24.8%)
> Residents with no health insurance: 10.9% (state: 10.1%)
> Median household income: $59,779 (state: $62,087)
Certain unhealthy habits are more common in Wichita than in any other metro area in the state. For example, 26.0% of adults do not exercise regularly, the largest share of the four metro areas in Kansas. Unhealthy lifestyles may be taking a toll, as 34.0% of adults in Wichita are obese, compared to 33.2% across Kansas.
Unemployment is associated with increased risk of unhealthy behaviors such as tobacco and alcohol consumption and poor diet and an increased risk of premature mortality overall. In Wichita, the annual unemployment rate stands at 3.4%, higher than every other metro area in Kansas and slightly higher than the state jobless rate of 3.2%.
[in-text-ad]

Kentucky: Bowling Green
> Adult obesity rate: 31.4% (state: 33.8%)
> Adult smoking rate: 20.5% (state: 24.6%)
> Pct. of adults who don’t exercise: 26.2% (state: 28.6%)
> Residents with no health insurance: 7.4% (state: 6.4%)
> Median household income: $51,198 (state: $52,295)
People living in urban areas tend to have healthier behaviors and better health outcomes than those living in rural areas. So while Bowling Green is the least healthy city in Kentucky, it is still healthier than the population of the relatively rural state as a whole by several measures.
For example, 20.5% of Bowling Green residents smoke, less than the smoking rate of 24.6% statewide.
Additionally, 31.4% of Bowling Green adults are obese, compared to the state obesity rate of 33.8%. Overall, 433 in every 100,000 Bowling Green residents die before the age of 75, the third highest premature death rate of any metro area in Kentucky and higher than the national average of 340 premature deaths per 100,000 people, yet less than the state rate of 475 per 100,000.
Louisiana: Hammond
> Adult obesity rate: 38.7% (state: 35.4%)
> Adult smoking rate: 22.0% (state: 23.1%)
> Pct. of adults who don’t exercise: 33.7% (state: 29.2%)
> Residents with no health insurance: 10.1% (state: 9.6%)
> Median household income: $47,825 (state: $51,073)
Hammond is the least healthy of the nine metro areas in Louisiana. Smoking is the leading cause of preventable death in the United States. And though the smoking rate of 22.0% in Hammond is lower than the state smoking rate of 23.1%, it is the second highest among metro areas in the state.
Hammond residents are also more likely to lead physically inactive lifestyles than those in any other metro area in the state. About 33.7% of adults in Hammond report no leisure-time physical activity, the 11 highest share of all 381 metro areas in the U.S. For context, the physical inactivity rate in Louisiana is 29.2%, and the national rate is 23.0%.

Maine: Bangor
> Adult obesity rate: 33.7% (state: 29.9%)
> Adult smoking rate: 16.9% (state: 17.3%)
> Pct. of adults who don’t exercise: 23.5% (state: 21.6%)
> Residents with no health insurance: 10.9% (state: 10.2%)
> Median household income: $50,449 (state: $58,924)
About 23.5% of adults in the Bangor metro area do not regularly engage in physical activity, compared to 21.6% of adults across the state. Regular exercise can help in maintaining a healthy weight, and 33.7% of adults in Bangor are obese, compared to 29.9% of adults across the state. Exercise and other healthy behaviors can also help lower the risk of premature death. In Bangor, some 379 in every 100,000 residents die before the age of 75, more than the statewide rate of 337 per 100,000.
People with health insurance are more likely to get screened for health problems because they do not have to pay the prohibitively high prices of such tests, and often, the earlier a disease is caught, the better the chances of successful treatment. Bangor has the state’s highest uninsured rate at 10.9%, higher than the statewide and nationwide rates of 10.2% and 10.0%, respectively.
[in-text-ad-2]

Maryland: Cumberland
> Adult obesity rate: 36.4% (state: 31.0%)
> Adult smoking rate: 17.5% (state: 13.8%)
> Pct. of adults who don’t exercise: 27.9% (state: 22.4%)
> Residents with no health insurance: 6.2% (state: 7.0%)
> Median household income: $49,729 (state: $86,738)
Cumberland is the least healthy of the five metro areas in Maryland. The smoking rate in the city is 17.5%, higher than both the state smoking rate of 13.8% and the national rate of 17.0%. Smoking is one of the leading causes of preventable death in the United States, and in Cumberland, there are 434 premature deaths annually for every 100,000 people, well above the state rate of 339 per 100,000.
Lower-income Americans do not have access to as many health care options as those with higher incomes, and they are less able to afford leading a healthy lifestyle. In Cumberland, the typical household earns just $49,729 a year. Meanwhile, the typical Maryland household earns nearly $87,000 annually.

Massachusetts: Springfield
> Adult obesity rate: 29.2% (state: 24.7%)
> Adult smoking rate: 14.9% (state: 13.7%)
> Pct. of adults who don’t exercise: 23.4% (state: 21.3%)
> Residents with no health insurance: 3.4% (state: 3.3%)
> Median household income: $62,346 (state: $85,843)
Springfield is the least healthy of the five metro areas in Massachusetts. Some 16.8% of metro area adults in the city report being in fair or poor health, a larger share than in every other metro area in the state and well above the 14.4% share of adults across Massachusetts as a whole.
The prevalence of low self-reported health status in Springfield is likely attributable in part to unhealthy lifestyles. Adults in Springfield are more likely to lead sedentary lives and more likely to smoke than adults in every other metro area in the state.
[in-text-ad]

Michigan: Flint
> Adult obesity rate: 34.9% (state: 32.0%)
> Adult smoking rate: 19.0% (state: 19.3%)
> Pct. of adults who don’t exercise: 26.2% (state: 23.4%)
> Residents with no health insurance: 6.7% (state: 6.1%)
> Median household income: $50,389 (state: $59,584)
Low birthweight can be indicative of unhealthy maternal lifestyles, limited access to health care, and other negative environmental factors. Flint is the only metro area in Michigan where over 10% of newborns weigh below what is considered a healthy weight, one of the highest shares of any metro area in the country. Flint also has the highest premature death rate among metro areas in the state, with 479 deaths before age 75 annually for every 100,000 people.
Those who are unemployed are more likely to have unhealthy behaviors and report worse health outcomes than those who are employed. In Flint, the annual unemployment rate stands at 4.9%, the highest of any metro area in the state.

Minnesota: Duluth
> Adult obesity rate: 29.0% (state: 27.9%)
> Adult smoking rate: 17.3% (state: 14.5%)
> Pct. of adults who don’t exercise: 21.5% (state: 20.1%)
> Residents with no health insurance: 5.4% (state: 5.1%)
> Median household income: $60,316 (state: $74,593)
Smoking — the leading cause of preventable death in the United States — is relatively common in Duluth, as 17.3% of adults are smokers, the largest share of any metro area in Minnesota. Duluth has the highest premature death rate in the state at 333 deaths per 100,000 people, significantly higher than the state average of 266 deaths per 100,000 people.
People with health insurance are more likely to get screened for different health problems because they do not have to pay prohibitively high out-of-pocket prices for tests, and the earlier the disease is caught, the better. About 5.4% of Duluth residents lack health insurance, more than any other metro area in the state.

Mississippi: Gulfport-Biloxi-Pascagoula
> Adult obesity rate: 33.5% (state: 36.8%)
> Adult smoking rate: 20.4% (state: 22.2%)
> Pct. of adults who don’t exercise: 29.3% (state: 31.9%)
> Residents with no health insurance: 15.1% (state: 14.5%)
> Median household income: $50,642 (state: $45,792)
Gulfport-Biloxi-Pascagoula ranks as the least healthy metro area in Mississippi. About 15.1% of adult residents are uninsured, more than the state uninsured rate of 14.5% and more than any other metro area in Mississippi. Residents of Gulfport-Biloxi-Pascagoula report 4.4 mentally unhealthy days a month, more than the other two metro areas in the state but slightly less than the state average of 5.0 days a month.
People living in Gulfport-Biloxi-Pascagoula are more likely to practice certain unhealthy habits. The 20.4% smoking rate in Gulfport is the highest of any metro area in the state and one of the highest in the country, yet below the 22.2% statewide smoking rate.
[in-text-ad-2]

Missouri: St. Joseph
> Adult obesity rate: 37.4% (state: 32.2%)
> Adult smoking rate: 20.8% (state: 20.8%)
> Pct. of adults who don’t exercise: 30.9% (state: 25.8%)
> Residents with no health insurance: 11.0% (state: 10.9%)
> Median household income: $50,425 (state: $57,409)
Some 37.4% of adults in the St. Joseph metro area are obese, the largest share of any metro area in Missouri. Additionally, 20.8% of adults smoke, also the largest share in the state. Unhealthy lifestyles can contribute to poor health outcomes, and about one in every five adults in St. Joseph report being in fair or poor health — the largest share of any metro area in Missouri and above both the 18.0% state and 17.0% national rates.
Adults in St. Joseph are also less likely to exercise than the typical adult in the state. The prevalence of sedentary lifestyles may be partially attributable to a lack of exercise opportunities in the metro area. Just 74.9% of the metro population has access to places for physical activity like parks and recreation centers — below the 76.7% share of state residents and 84.0% of Americans nationwide who do.

Montana: Great Falls
> Adult obesity rate: 27.3% (state: 25.8%)
> Adult smoking rate: 16.8% (state: 17.2%)
> Pct. of adults who don’t exercise: 24.5% (state: 21.6%)
> Residents with no health insurance: 10.1% (state: 10.4%)
> Median household income: $51,227 (state: $57,153)
Of the three metro areas in Montana, Great Falls is the least healthy. Adults in Great Falls are the least likely to exercise and are most likely to be obese than residents of any other metro area in the state. Adults in Great Falls also have more mentally and physically unhealthy days a month than adults in the other two metro areas in Montana.
Uninsured adults are less likely to receive preventative medical care than adults with health insurance, and they are more likely to suffer negative health consequences such as preventable hospitalization as a result. In Great Falls, 10.1% of adults under age 65 lack health insurance, the largest uninsured rate in Montana. Additionally, there are 3,455 preventable hospitalizations per 100,000 Medicare enrollees in Great Falls, the highest rate of any metro area in the state.
[in-text-ad]

Nebraska: Grand Island
> Adult obesity rate: 35.0% (state: 32.2%)
> Adult smoking rate: 15.3% (state: 15.4%)
> Pct. of adults who don’t exercise: 27.9% (state: 23.3%)
> Residents with no health insurance: 12.1% (state: 9.6%)
> Median household income: $55,907 (state: $63,229)
Obesity is a risk factor for a number of potentially fatal diseases and conditions, including heart disease, diabetes, and certain cancers. The adult obesity rate of 35.0% in Grand Island is higher than the state obesity rate of 32.2% and higher than the obesity rate in the two other metro areas in Nebraska — Omaha-Council Bluffs and Lincoln. The premature death rate in Grand Island of 326 deaths before age 75 for every 100,000 people is also higher than the statewide rate of 310 premature deaths per 100,000 Nebraska residents.
Lower-income households cannot afford as many healthy options related to health care, diet, and lifestyle as wealthy households, and as a result they often report worse health outcomes. In Grand Island, 7.7% of households live on less than $10,000 a year, the largest share of any Nebraska metro area and higher than the statewide share of 4.8%.
Nevada: Carson City
> Adult obesity rate: 28.3% (state: 25.7%)
> Adult smoking rate: 19.0% (state: 17.6%)
> Pct. of adults who don’t exercise: 22.3% (state: 23.1%)
> Residents with no health insurance: 12.6% (state: 13.1%)
> Median household income: $57,270 (state: $63,276)
Carson City has far and away the highest premature death rate of any metro area in Nevada. There are 499 deaths before age 75 for every 100,000 people in the metro area annually, significantly higher than the state premature death rate of 364 per 100,000.
Smoking is the leading cause of preventable death in the United States. In Carson City, 19.0% of adults smoke, higher than the 17.6% state smoking rate. Obesity is also a risk factor for a number of potentially deadly diseases and conditions, including stroke, diabetes, and certain cancers, and Carson City’s 28.3% obesity rate is the highest of the three metro areas in Nevada.

New Hampshire: Manchester-Nashua
> Adult obesity rate: 28.0% (state: 27.9%)
> Adult smoking rate: 13.5% (state: 15.7%)
> Pct. of adults who don’t exercise: 22.5% (state: 21.3%)
> Residents with no health insurance: 7.2% (state: 7.0%)
> Median household income: $83,626 (state: $77,933)
Manchester is the only metro area in New Hampshire and therefore ranks as the least healthy by default. Still, Manchester is slightly worse off than the state as a whole in a number of health outcomes. For example, Manchester’s premature death rate of 313 deaths before age 75 per 100,000 people is slightly higher than the state rate of 308 per 100,000.
Despite the poorer health outcomes, Manchester residents are more likely to exhibit certain healthy habits than the typical New Hampshire resident. Just 13.5% of metro area adults smoke, and 20.2% drink excessively, compared to 15.7% and 20.7% of adults statewide, respectively.
[in-text-ad-2]

New Jersey: Vineland-Bridgeton
> Adult obesity rate: 35.9% (state: 26.4%)
> Adult smoking rate: 18.3% (state: 13.7%)
> Pct. of adults who don’t exercise: 31.2% (state: 26.0%)
> Residents with no health insurance: 12.1% (state: 9.0%)
> Median household income: $54,587 (state: $85,751)
In Vineland-Bridgeton, 22.6% of adults report being in fair or poor health, by far the largest share of any of the state’s four metro areas and well above the 17.7% share of adults who report similar health outcomes across New Jersey as a whole.
Poor health status among area adults may be partially attributable to unhealthy lifestyles. Just 68.8% of adults in the Vineland metro exercise regularly, the smallest share in New Jersey. Adults in Vineland are also more likely to smoke and be obese than than the average adult in the state.

New Mexico: Farmington
> Adult obesity rate: 33.2% (state: 26.6%)
> Adult smoking rate: 21.6% (state: 17.5%)
> Pct. of adults who don’t exercise: 23.9% (state: 19.7%)
> Residents with no health insurance: 14.0% (state: 11.0%)
> Median household income: $44,321 (state: $51,945)
Residents of Farmington report among the most mentally and physically unhealthy days not just in New Mexico but the entire country. City adults report an average of 5.2 physically unhealthy days a month, the highest in the state and second highest of all 381 metro areas. Adults report an average of 4.9 mentally unhealthy days per month, the highest in the state and 19th highest in the U.S. With an obesity rate of 33.2%, the metro area also has far and away the largest share of adults who are dangerously overweight.
Unhealthy lifestyles may contribute to such unhealthy outcomes. Regular exercise can be good for mental health and help in maintaining a healthy weight. In Farmington, 23.9% of adults don’t exercise regularly, by far the largest share of any metro area in the state and well above the 19.7% of adults across the state who lead sedentary lives.
[in-text-ad]

New York: Buffalo-Cheektowaga-Niagara Falls
> Adult obesity rate: 30.8% (state: 25.5%)
> Adult smoking rate: 17.2% (state: 14.1%)
> Pct. of adults who don’t exercise: 26.3% (state: 24.7%)
> Residents with no health insurance: 4.6% (state: 6.6%)
> Median household income: $60,105 (state: $72,108)
Smoking is a leading cause of preventable death in the United States, and the adult smoking rate of Buffalo-Cheektowaga-Niagara Falls is 17.2%, the highest of New York’s 12 metro areas. Regular and excessive consumption of alcohol can result in chronic conditions and other long-term health problems, such as high blood pressure, heart disease, stroke, liver disease, and certain cancers. About 22.2% of adults in the metro area report excessive drinking, more than any other metro area in the state and higher than the national rate of 19.0%.
Low-income Americans have less access to quality health care options than those with higher incomes, and they are less able to afford living a healthy lifestyle. In the Buffalo metro area, the typical household earns $60,105 a year, compared to the state median of $72,108.

North Carolina: Rocky Mount
> Adult obesity rate: 40.6% (state: 31.4%)
> Adult smoking rate: 19.2% (state: 17.2%)
> Pct. of adults who don’t exercise: 29.8% (state: 24.3%)
> Residents with no health insurance: 12.2% (state: 12.6%)
> Median household income: $46,466 (state: $57,341)
Rocky Mount is the least healthy metro area in North Carolina and also among the least healthy in the nation. Rocky Mount’s premature death rate of 505 deaths before age 75 for every 100,000 people is by far the highest of the 15 metro areas in North Carolina and the 16th highest in the nation. It is also far higher than the state premature death rate of 372 per 100,000 or the national rate of 340 premature deaths per 100,000.
The higher premature death rate in the metro area is likely due in part to the prevalence of some unhealthy behaviors and outcomes. For example, 40.6% of metro area adults are obese, the largest share of any metro area in the state and the seventh highest obesity rate of all 381 metro areas. Obesity is a risk factor for a number of potentially deadly diseases and conditions, including diabetes, heart disease, and certain cancers.

North Dakota: Grand Forks
> Adult obesity rate: 34.0% (state: 32.7%)
> Adult smoking rate: 15.9% (state: 18.3%)
> Pct. of adults who don’t exercise: 24.2% (state: 23.9%)
> Residents with no health insurance: 7.3% (state: 8.6%)
> Median household income: $57,301 (state: $64,577)
People living in urban areas tend to have healthier behaviors and better health outcomes than residents of rural areas. While Grand Forks ranks as the least healthy metro area in North Dakota, it performs better than the largely rural state as a whole in several measures.
For example, 15.9% of adults in Grand Forks smoke, less than the 18.3% state smoking rate. Adults who do not smoke and are normal weight are less likely to self-report being in poor health, and in Grand Forks, 14.5% of adults report being in fair or poor health, less than the 15.1% of adults who do statewide and the 17.0% who do nationwide.
[in-text-ad-2]

Ohio: Springfield
> Adult obesity rate: 33.7% (state: 32.3%)
> Adult smoking rate: 21.4% (state: 21.1%)
> Pct. of adults who don’t exercise: 30.5% (state: 26.4%)
> Residents with no health insurance: 7.2% (state: 7.1%)
> Median household income: $50,128 (state: $58,642)
Springfield is the only metro area in Ohio where adults report an average of 4.5 physically unhealthy days per month, the most of all 11 metro areas in the state. Springfield residents are also more likely than those in any other Ohio metro areas to die prematurely. There are 551 deaths before age 75 for every 100,000 metro area residents annually, compared to the statewide premature death rate of 408 per 100,000.
Poor health outcomes are partially attributable to unhealthy lifestyles. For example, adults in Springfield are more likely to smoke than adults across the state. Springfield’s 21.4% adult smoking rate is the highest of all metro areas in Ohio and the 14th highest of all 381 U.S. metro areas.

Oklahoma: Lawton
> Adult obesity rate: 32.6% (state: 33.7%)
> Adult smoking rate: 19.5% (state: 20.1%)
> Pct. of adults who don’t exercise: 30.2% (state: 29.3%)
> Residents with no health insurance: 15.1% (state: 16.5%)
> Median household income: $51,332 (state: $54,449)
Some 17.8% of residents in the Lawton metro area live below the poverty line, the highest poverty rate of any city in Oklahoma and higher than the state poverty rate of 15.2%. Income is one of the largest determinants of health, and areas with higher poverty rates tend to have worse health behaviors and outcomes.
In Lawton, 19.5% of adults smoke, the highest smoking rate of any Oklahoma metro area. Just 69.8% of adults regularly exercise, less than the 70.7% state activity rate. Tobacco use and inactivity are two of the leading causes of premature death, and in Lawton, 465 in every 100,000 residents die before the age of 75 — the highest premature death rate in Oklahoma and among the highest of any city in the country.
[in-text-ad]
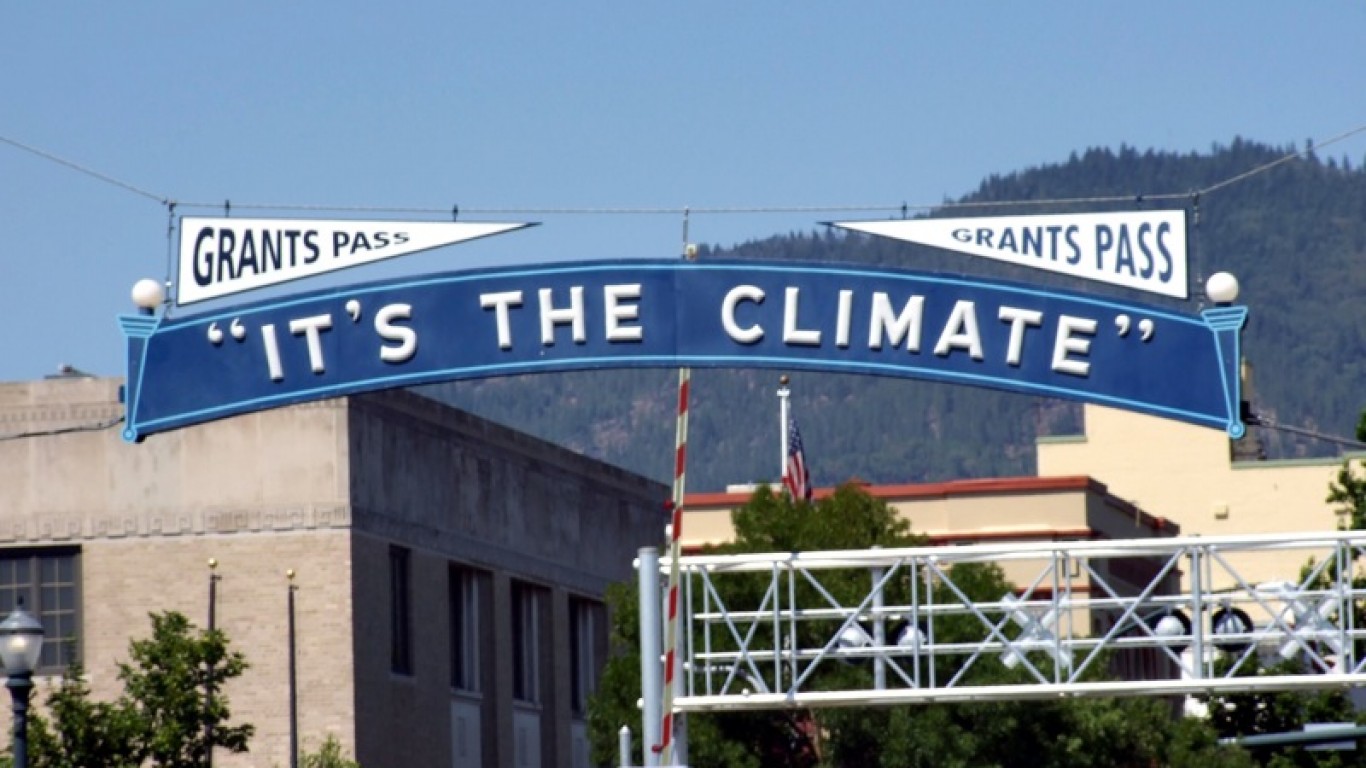
Oregon: Grants Pass
> Adult obesity rate: 31.1% (state: 28.8%)
> Adult smoking rate: 17.0% (state: 16.1%)
> Pct. of adults who don’t exercise: 20.7% (state: 17.2%)
> Residents with no health insurance: 8.5% (state: 8.2%)
> Median household income: $47,573 (state: $67,058)
The premature death rate in Grants Pass is 431 per 100,000 people, significantly higher than the statewide premature death rate of 304 per 100,000 and the highest in all eight metro areas in Oregon. Adults in Grants Pass are more likely to report being in poor mental health than the average Oregon resident.
Low-income households cannot afford as many healthy options related to health care, diet, and lifestyle as wealthier households, and they often report worse health outcomes as a result. In Grants Pass, the typical household earns just $47,573 a year, well below the $67,058 state median.

Pennsylvania: Scranton–Wilkes-Barre–Hazleton
> Adult obesity rate: 29.6% (state: 30.3%)
> Adult smoking rate: 19.6% (state: 18.7%)
> Pct. of adults who don’t exercise: 27.6% (state: 23.1%)
> Residents with no health insurance: 6.4% (state: 6.6%)
> Median household income: $54,304 (state: $63,463)
Scranton–Wilkes-Barre–Hazleton is among the least healthy metro areas not just in Pennsylvania but the entire country. About 27.6% of area adults live a sedentary lifestyle, the second highest share in the state and well above the state inactivity rate of 23.1%. The area’s adult smoking rate of 19.6% is also the second highest in the state.
Scranton–Wilkes-Barre–Hazleton has the second highest premature death rate of any of the 18 metro areas in Pennsylvania. There are 427 deaths before age 75 annually for every 100,000 metro area residents, well above the state premature death rate of 359 per 100,000.

Rhode Island: Providence-Warwick
> Adult obesity rate: 28.5% (state: 28.1%)
> Adult smoking rate: 14.3% (state: 14.9%)
> Pct. of adults who don’t exercise: 25.2% (state: 24.4%)
> Residents with no health insurance: 4.8% (state: 5.4%)
> Median household income: $70,967 (state: $71,169)
The Providence-Warwick metro area encompasses nearly all of Rhode Island as well as Bristol County in Massachusetts. As the only metro area in Rhode Island, Providence ranks as the least healthy city in the state by default and matches the state as a whole in most measures of health behaviors and outcomes. For example, 28.5% of adults in Providence are obese, compared to 28.1% of adults across the state. Similarly, 14.3% of adults in Providence report smoking, closely in line with the 14.9% of adults who smoke throughout Rhode Island.
[in-text-ad-2]

South Carolina: Florence
> Adult obesity rate: 37.9% (state: 32.9%)
> Adult smoking rate: 18.3% (state: 18.8%)
> Pct. of adults who don’t exercise: 32.0% (state: 25.9%)
> Residents with no health insurance: 11.7% (state: 13.1%)
> Median household income: $48,547 (state: $56,227)
Florence is the least healthy metro area in South Carolina and among the least healthy in the U.S. Only 68.0% of adults in the Florence metro area get regular exercise, a smaller share than the 74.1% of adults across South Carolina. Remaining active can help in maintaining a healthy weight, and in Florence, 37.9% of adults are obese, compared to 32.9% of adults statewide.
Obesity is a risk factor for a number of potentially deadly diseases and conditions, including diabetes, heart disease, and certain cancers. In Florence, there are 534 deaths before age 75 for every 100,000 people annually, more than any of the eight metro areas in the state and well above the state premature death rate of 413 per 100,000.

South Dakota: Rapid City
> Adult obesity rate: 28.8% (state: 31.8%)
> Adult smoking rate: 16.0% (state: 19.3%)
> Pct. of adults who don’t exercise: 19.9% (state: 21.3%)
> Residents with no health insurance: 11.4% (state: 10.8%)
> Median household income: $58,361 (state: $59,533)
Of the two metro areas in South Dakota — Sioux Falls and Rapid City — Rapid City is the least healthy. Unlike in Sioux Falls, adults in Rapid City report more than three physically unhealthy days and more than three mentally unhealthy days per month on average.
Some 13.4% of adults in Rapid City report being in fair or poor health, more than the 11.1% of adults who report similar health outcomes in Sioux Falls and in line with the share of adults in fair or poor health statewide. For every 100,000 Rapid City residents, 323 die before the age of 75 — more than the Sioux Falls premature death rate of 290 per 100,000, yet less than the state rate of 333 per 100,000.
[in-text-ad]

Tennessee: Memphis
> Adult obesity rate: 35.9% (state: 33.2%)
> Adult smoking rate: 19.5% (state: 22.6%)
> Pct. of adults who don’t exercise: 27.0% (state: 27.2%)
> Residents with no health insurance: 11.5% (state: 11.3%)
> Median household income: $54,859 (state: $56,071)
Low birthweight can be indicative of unhealthy maternal lifestyles, limited access to health care, and other negative environmental factors. In Memphis, 11.3% of newborns weigh less than what is considered a healthy weight, compared to 9.2% of newborns across the state as a whole.
Living below the poverty line can greatly reduce an individual’s ability to access health care and make healthy lifestyle choices, and as a result, poorer Americans often report worse health outcomes. In Memphis, 15.4% of residents live below the poverty line, compared to 13.9% of the Tennessee population.
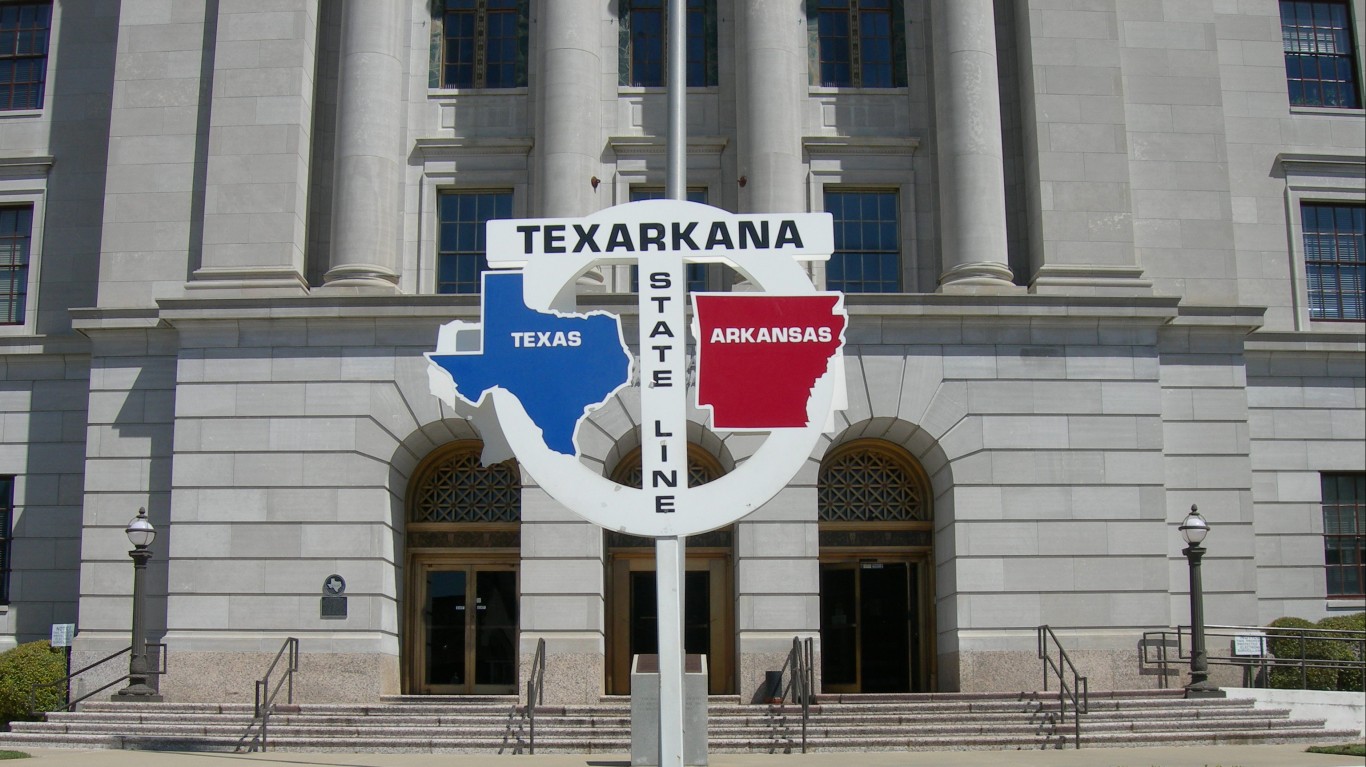
Texas: Texarkana
> Adult obesity rate: 43.6% (state: 30.1%)
> Adult smoking rate: 18.7% (state: 15.7%)
> Pct. of adults who don’t exercise: 39.2% (state: 24.4%)
> Residents with no health insurance: 13.3% (state: 19.4%)
> Median household income: $51,544 (state: $64,034)
In Texarkana, Texas, 43.6% of adults are obese, well above the state obesity rate of 30.1% and the highest obesity rate of all metro areas not only in Texas but the entire country. Obesity is a risk factor for a number of potentially deadly diseases and conditions, including diabetes, heart disease, and certain cancers, and premature death is far more common in Texarkana than it is across the state as a whole. For every 100,000 people in the metro area, there are 507 deaths before age 75 annually, the highest premature death rate of all 25 metro areas in the state and the 12th highest in the U.S.

Utah: Salt Lake City
> Adult obesity rate: 25.2% (state: 25.9%)
> Adult smoking rate: 9.6% (state: 8.9%)
> Pct. of adults who don’t exercise: 18.2% (state: 18.1%)
> Residents with no health insurance: 10.8% (state: 10.0%)
> Median household income: $80,196 (state: $75,780)
Of Utah’s five metro areas, Salt Lake City is the least healthy. Part of the reason may be environmental. The air in Salt Lake City has the highest concentration of harmful particulate matter of any metro area in the state. Still, Salt Lake City’s air is slightly cleaner than average on a national scale.
Adults in Salt Lake City are also more likely than those in every other metro area in the state to have certain unhealthy habits. For example, 15.6% of adults in the city drink excessively, higher than the excessive drinking rate of 12.2% statewide.
[in-text-ad-2]

Vermont: Burlington-South Burlington
> Adult obesity rate: 25.6% (state: 26.3%)
> Adult smoking rate: 12.8% (state: 15.8%)
> Pct. of adults who don’t exercise: 17.2% (state: 19.1%)
> Residents with no health insurance: 5.0% (state: 5.5%)
> Median household income: $74,909 (state: $63,001)
Burlington is the only metro area in Vermont, and as a result it ranks as the least healthy city in the state by default only. In fact, by several measures, city residents are more likely to have healthier lifestyles and report better health outcomes than those living across the state as a whole. For example, just 12.8% of adults in Burlington smoke, compared to 15.8% of the adult population in Vermont as a whole. Adults in Burlington are also more likely to regularly exercise and are less likely to be obese than the typical adult in the state.
Healthy behaviors can lead to healthy outcomes, and in Burlington, adult residents report an average of 3.2 physically unhealthy days per month, compared to an average of about 3.6 days per month across the state.

Virginia: Lynchburg
> Adult obesity rate: 36.0% (state: 29.8%)
> Adult smoking rate: 16.7% (state: 16.4%)
> Pct. of adults who don’t exercise: 28.9% (state: 22.9%)
> Residents with no health insurance: 10.7% (state: 10.2%)
> Median household income: $57,736 (state: $76,456)
Lynchburg’s adult obesity rate of 36.0% is higher than in any other metro area in Virginia. Adult residents of Lynchburg are more likely to lead a sedentary lifestyle than adults living across the state. About 28.9% report they do not exercise regularly, compared to 22.9% of adults statewide.
Smoking is the leading cause of preventable death in the United States, and in Lynchburg, 16.7% of adults are smokers, compared to 16.4% of adults across the state.
[in-text-ad]
Washington: Yakima
> Adult obesity rate: 34.9% (state: 27.8%)
> Adult smoking rate: 14.4% (state: 13.5%)
> Pct. of adults who don’t exercise: 22.7% (state: 17.0%)
> Residents with no health insurance: 12.9% (state: 7.1%)
> Median household income: $56,233 (state: $78,687)
In Yakima, Washington, 23.5% of adults report being in fair or poor health, by far the largest share of any metro area in the state and the 11th highest share in the country. For context, 17.0% of adults in the U.S. and 15.6% of adults across Washington state report similar health outcomes.
Living with serious financial hardship can lower access to health care options as well as reduce the ability to make healthier lifestyle choices, and as a result, poorer Americans often report worse health outcomes. In Yakima, 16.9% of residents live below the poverty line, compared to the state poverty rate of 9.8%.

West Virginia: Beckley
> Adult obesity rate: 39.4% (state: 36.7%)
> Adult smoking rate: 24.7% (state: 26.0%)
> Pct. of adults who don’t exercise: 31.2% (state: 28.9%)
> Residents with no health insurance: 7.6% (state: 7.5%)
> Median household income: $44,785 (state: $48,850)
Beckley, West Virginia, has the highest premature death rate in the United States. There are 597 deaths before age 75 annually for every 100,000 people, more than the state rate of 502 per 100,000 and the national rate of 340 per 100,000. Smoking is the leading cause of preventable death in the United States, and in Beckley, 24.7% of adults smoke, the largest share of any metro area not only in West Virginia but in the country as a whole. The national smoking rate is 17.0%.
Those who are unemployed are more likely to have unhealthy behaviors and to report worse health outcomes than those who are employed. In Beckley, the annual unemployment rate was 5.0% in 2019, higher than the 4.9% rate across the state.

Wisconsin: Janesville-Beloit
> Adult obesity rate: 36.3% (state: 31.3%)
> Adult smoking rate: 17.3% (state: 16.0%)
> Pct. of adults who don’t exercise: 22.4% (state: 20.8%)
> Residents with no health insurance: 7.2% (state: 6.4%)
> Median household income: $61,243 (state: $64,168)
Janesville-Beloit is the least healthy metro area in Wisconsin and the fifth least healthy area among all 381 metro areas in the U.S. People with health insurance are more likely to get screened for different health problems because they do not have to pay prohibitively high out-of-pocket prices for tests, and the earlier the disease is caught, the better. About 7.2% of adults under 65 are uninsured, the highest share of all other metro areas in Wisconsin
Smoking is a leading cause of preventable death in the U.S. About 17.3% of adults in Janesville-Beloit smoke, the highest smoking rate of all metro areas in the state. Close to 355 in every 100,000 Janesville-Beloit area residents die before the age of 75 each year, more than the state premature death rate of 309 per 100,000 and the highest of any city in the state.
[in-text-ad-2]

Wyoming: Casper
> Adult obesity rate: 31.8% (state: 28.9%)
> Adult smoking rate: 17.8% (state: 18.7%)
> Pct. of adults who don’t exercise: 25.0% (state: 24.1%)
> Residents with no health insurance: 14.2% (state: 14.2%)
> Median household income: $65,034 (state: $65,003)
In Casper, Wyoming, there are 367 deaths before age 75 for every 100,000 people annually, a higher premature death rate than in Cheyenne — the only other metro area in the state — and across Wyoming as a whole.
Obesity is a risk factor for a number of potentially deadly diseases and conditions, including diabetes, heart disease, and certain cancers. In Casper, 31.8% of adults are obese, higher than the 28.9% state obesity rate and the 30.0% obesity rate in Cheyenne.
Methodology
To determine the least healthy city in every state, 24/7 Wall St. created an index composed of 35 health outcomes and health factors with data from the 2020 County Health Rankings & Roadmaps, a joint program of the Robert Wood Johnson Foundation and the University of Wisconsin Population Health Institute. We calculated composite scores for outcomes and factors separately, then combined the two scores to form a single score that determined the metropolitan statistical area’s rank.
All data used in the index came from the CHR with the exception of 2019 annual unemployment rates for each MSA — these are the most recent annual figures available from the Bureau of Labor Statistics’ Local Area Unemployment Statistics program. For all other CHR measures, county-level data was aggregated to the MSA level using raw values provided at the county level, and measures without raw values by county were calculated using weighted averages based on population distribution within each MSA by county.
We also considered measures from the American Community Survey (ACS) including median household income, poverty and educational attainment rates. These measures were not included in the index.
Values selected for the index were standardized into Z-Scores, which assumes a mean of 0 and a standard deviation of 1. Z-scores are calculated for each index measure by MSA, within each of their respective states. If an MSA spans multiple states, then the city was indexed according to its primary state, as designated by the Census Bureau. Note that four states — Rhode Island, New Hampshire, Vermont, and Delaware — only have one MSA.
Health outcomes with the heaviest weights in the index include the age-adjusted premature mortality rate, the percentage of births with low birthweight, the percentage of adults reporting fair or poor health, and the age-adjusted average number of mentally and physically unhealthy days per month. The premature mortality rate is defined as the number of deaths under the age of 75 per 100,000 people. Unhealthy days are determined by the average number of days out of the month the adult population (18+) self-identifies as being unwell. This is used as an indicator of how chronic disabilities or illnesses (physical and mental) affect members of a particular geography.
Health factors with the heaviest weights in the index include the smoking rate, the 2019 annual unemployment rate, injury mortality, and the child poverty rate. Injury mortality per 100,000 measures the rate at which the total population is killed due to injury, whether intentional (for example suicide), or unintentional (drug overdose, car accidents, accidental suffocation, etc). Air Quality is another health factor and is determined by measuring the average daily density of particulate matter at 2.5 micrograms (or PM2.5 for short).
The remaining measures included in the index, as well as an explanation as to why they were used, can be found at County Health Rankings & Roadmaps.
Are you ready for retirement? Planning for retirement can be overwhelming, that’s why it could be a good idea to speak to a fiduciary financial advisor about your goals today.
Start by taking this retirement quiz right here from SmartAsset that will match you with up to 3 financial advisors that serve your area and beyond in 5 minutes. Smart Asset is now matching over 50,000 people a month.
Click here now to get started.
Thank you for reading! Have some feedback for us?
Contact the 24/7 Wall St. editorial team.