
This post may contain links from our sponsors and affiliates, and Flywheel Publishing may receive
compensation for actions taken through them.
The opioid epidemic is an ever-growing struggle, and the COVID-19 pandemic has made it even worse. Many Americans are anxious, stressed, isolated, and worried about their job and money — all risk factors for people who are already struggling with a substance-use disorder. The Centers for Disease Control and Prevention recently reported a record number of overdose deaths in a 12-mont period — 81,000 between June 2019 and May 2020.
Even before the pandemic, drug overdoses have been a leading cause of accidental death in the United States. More Americans die of drug overdoses than in car accidents, which are also frequently the result of substance abuse — nearly half of fatal car accidents involve alcohol or other substances. To better understand the likelihood of Americans dying from using a specific substance, it is important to also get a better understanding of the substance itself — its properties, interactions with other drugs and alcohol, and how often it is used.
The vast majority of people who drink alcohol in the United States — more than half of Americans — do so responsibly. Millions of people also use pain medication every day and do not stray from their prescribed dosage. And while overdoses from prescription opioids are a major factor in the opioid epidemic, opioids are essential to many Americans who rely on them to function.
The double-edged sword of risk and reward in prescribing opiates is common to many other drugs as well. Approximately half of all people in the United States use at least one prescription drug on a regular basis.
24/7 Tempo reviewed 25 of the most dangerous drugs and drug mixtures based on side effects and death rates tracked by the federal government, as well as potential risk of drug combinations measured by medical information organizations and web sources such as MedScape, WebMD, and the American Medical Association. These substances span well-known controlled substances, infamous street drugs produced in unsafe conditions, and lethal combinations of otherwise safe medications. Many of these drugs, when taken on their own and under the correct conditions, are considered to be generally safe. They are only seriously deadly when combined inappropriately with other drugs.
However, no drug is perfectly safe, and some widely-prescribed and popular over-the-counter medications are more likely to pose a risk to more Americans than rare drugs with a higher rates of dangerous side effects simply because they are more accessible. Some of the drugs on this list are a broad category of medication with similar effects and risks, while others are a single formula. According to doctors, opioids are not the only known effective pain treatment. Here is a list of nine non-opioid treatments approved by physicians.
Click here to see the 25 most dangerous drugs
Click here to read our detailed findings and methodology

1. Acetaminophen
> Common names/types: Tylenol, Mapap, Feverall
> Common uses: Pain relief
> Deadly when: Taken in excess, combined with alcohol, other pain meds containing acetaminophen
> Risks: Long-term liver damage, liver toxicity, death
[in-text-ad]

2. Alcohol
> Common names/types: Beer, wine, liquor
> Common uses: Recreation
> Deadly when: Combined with benzodiazepines, many other drugs
> Risks: Liver damage and failure, high blood pressure, death due to impaired motor functions
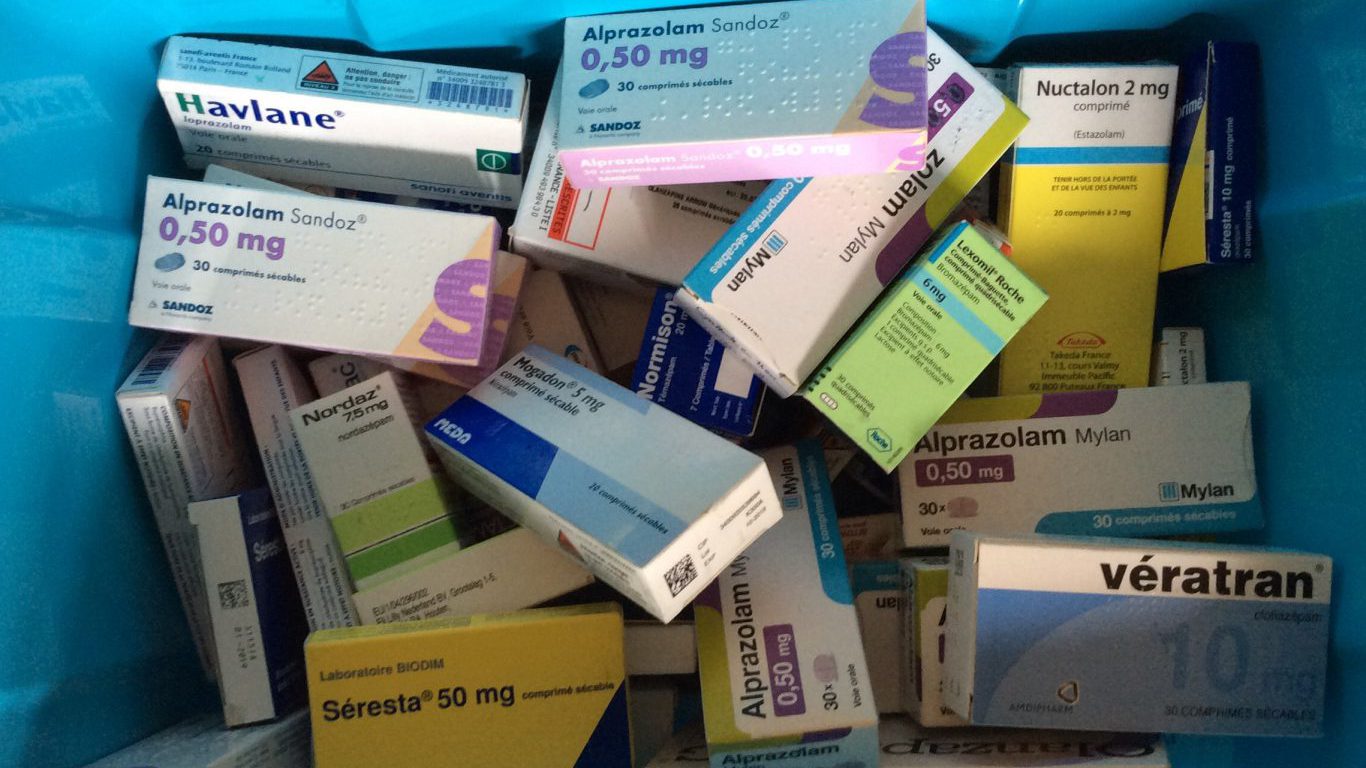
3. Anti-Anxiety Medication (benzodiazepines)
> Common names/types: Xanax, Valium, Klonopin
> Common uses: Anxiety treatment
> Deadly when: Combined with barbiturates, opioids, or alcohol
> Risks: Overdose, dementia

4. Anticoagulants
> Common names/types: Warfarin, Xarelto, Heparin
> Common uses: Blood clot risk
> Deadly when: Combined with Aspirin and other blood-thinning drugs
> Risks: Internal and external bleeding
[in-text-ad-2]

5. Antidepressants (SSRIs)
> Common names/types: Prozac, Lexapro, Paxil, Zoloft
> Common uses: Treatment of depression
> Deadly when: Other drugs that affect serotonin levels, opioids, NSAIDs
> Risks: Serotonin syndrome, suicide, internal bleeding

6. Anti-hypertensive Drugs
> Common names/types: Hytrin, Cardura, Minipress
> Common uses: High blood pressure
> Deadly when: Combined with NSAIDs and diuretics
> Risks: High blood pressure, acute renal failure, cerebrovascular complications
[in-text-ad]

7. Bromocriptine
> Common names/types: Parlodel, Cycloset
> Common uses: Tumors, Parkinson’s disease, type 2 diabetes
> Deadly when: Combined with pseudoephedrine (Sudafed)
> Risks: Bleeding in the stomach, seizures, death

8. Clarithromycin
> Common names/types: Clarithromycin
> Common uses: Antibiotic
> Deadly when: Combined with calcium channel blockers, statins like Lipitor
> Risks: Fatal heart complications

9. Clozapine
> Common names/types: Clozaril
> Common uses: Schizophrenia
> Deadly when: Combined with alcohol
> Risks: gastrointestinal hypomotility
[in-text-ad-2]

10. Cocaine
> Common names/types: Crack, coke, blow
> Common uses: Recreational stimulant, numbing agent
> Deadly when: Taken in excess, combined with heroin and opiates
> Risks: Death, heart attack, increased blood pressure

11. Colchicine
> Common names/types: Colcrys, Mitigare
> Common uses: Gout
> Deadly when: Combined with strong CYP3A4 Inhibitors
> Risks: Colchicine toxicity leading to death
[in-text-ad]

12. Cough Medicine
> Common names/types: NyQuil, Robitussin, Theraflu
> Common uses: Cough
> Deadly when: Combined with antihistamines
> Risks: Amplified sedative state leading to accidents
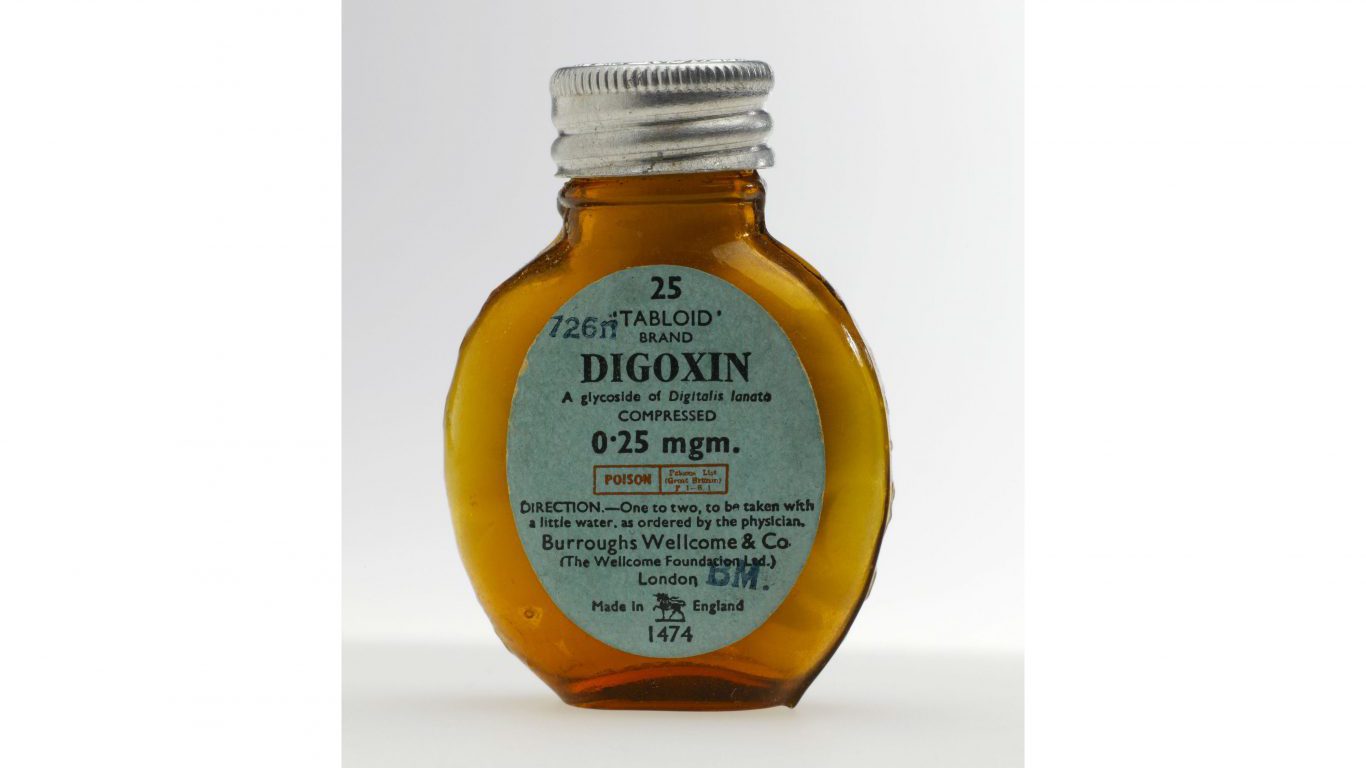
13. Digoxin
> Common names/types: Lanoxin
> Common uses: Heart conditions
> Deadly when: Combined with Quinidine
> Risks: Nausea, vomiting, death

14. Heroin and Semi-synthetic Opioids
> Common names/types: Percocet, Vicodin, Oxycontin
> Common uses: Pain relief
> Deadly when: Taken in excess, combined with cocaine and other drugs
> Risks: Accidental overdose
[in-text-ad-2]
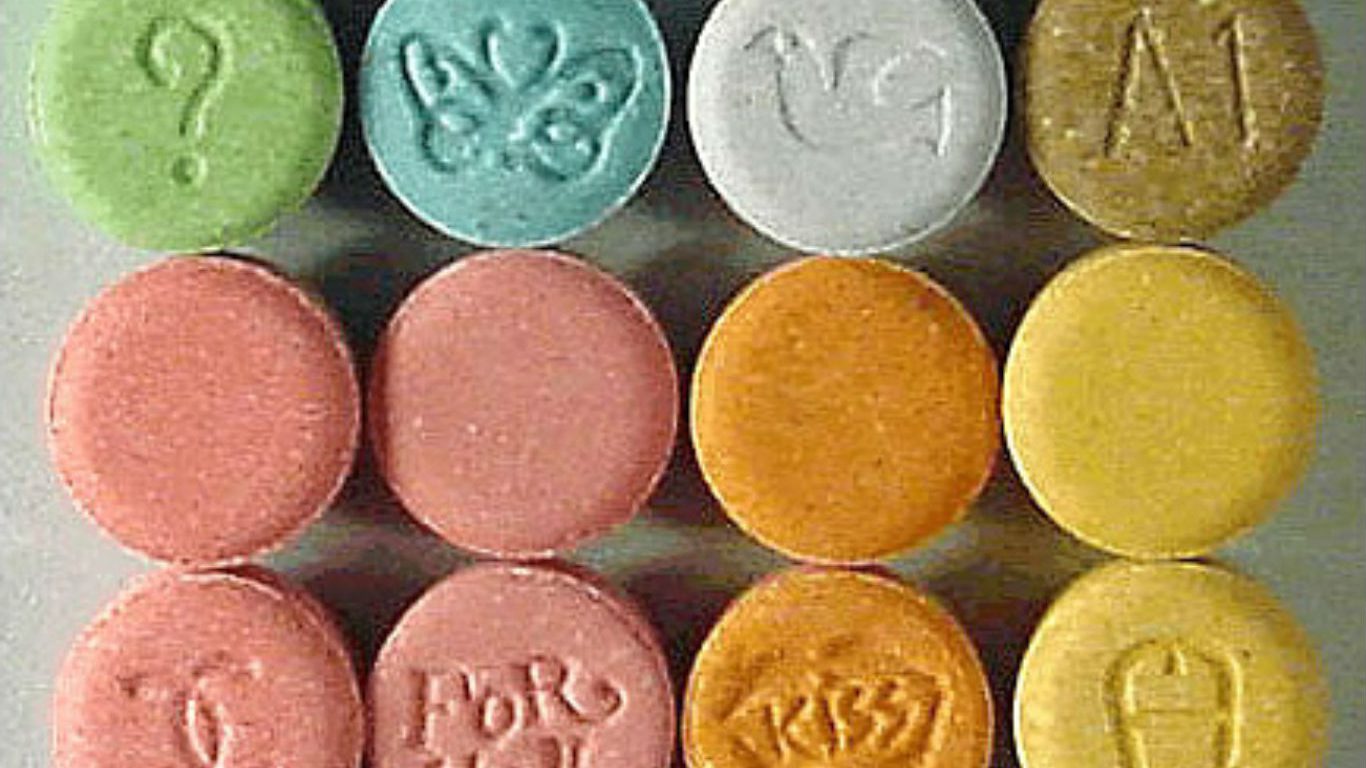
15. MDMA
> Common names/types: Ecstasy
> Common uses: Recreational euphoria
> Deadly when: Taken in excess, combined with alcohol, SSRIs
> Risks: Serotonin syndrome, shock, coma, death

16. Methamphetamine
> Common names/types: Crystal meth, Desoxyn
> Common uses: Stimulant
> Deadly when: Accidental overdose
> Risks: Teeth loss, brain damage, death
[in-text-ad]

17. Methotrexate
> Common names/types: Trexall, Rasuvo, Otrexup
> Common uses: Cancer, psoriasis, rheumatoid arthritis
> Deadly when: Taken too frequently, combined with Probenecid
> Risks: Liver, lung, or kidney damage, death
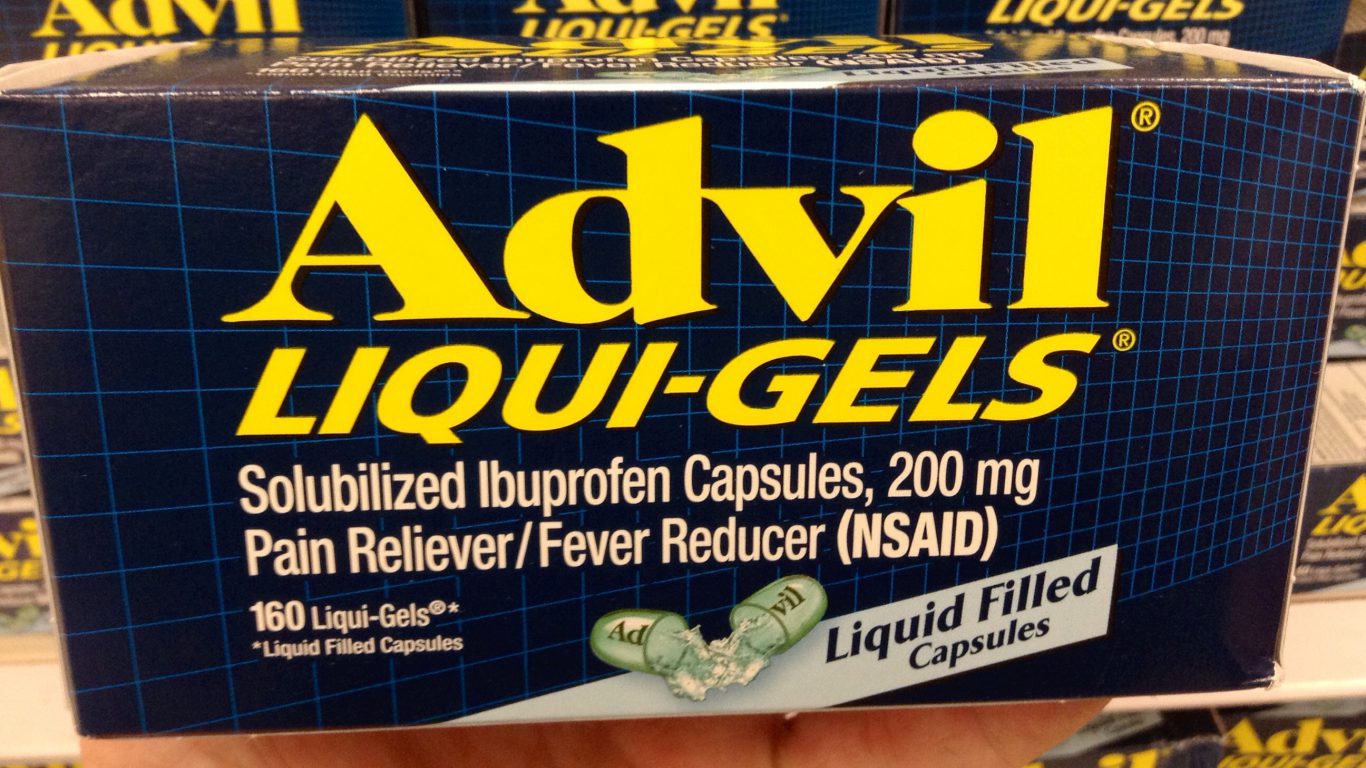
18. NSAIDs
> Common names/types: Advil, Aspirin, Ibuprofen
> Common uses: Pain relief, inflammation
> Deadly when: Combined with other blood-thinners
> Risks: Heart attack, stroke, Reye syndrome
19. Selective Serotonin Reuptake Inhibitors
> Common names/types: Celexa, Zoloft, Prozac, Lexapro
> Common uses: Depression
> Deadly when: Combined with other drugs that affect Serotonin levels
> Risks: Serotonin syndrome, increased risk of suicide
[in-text-ad-2]

20. Sildenafil
> Common names/types: Viagra, Revatio
> Common uses: Erectile dysfunction
> Deadly when: Combined with isosorbide mononitrate
> Risks: Death, dramatic blood pressure drop

21. Spironolactone
> Common names/types: Aldactone, CaroSpir
> Common uses: High blood pressure
> Deadly when: Combined with Potassium chloride
> Risks: hyperkalemia
[in-text-ad]

22. Statins
> Common names/types: Lipitor, Lescol, Crestor
> Common uses: Heart disease
> Deadly when: Combined with Fluconazole
> Risks: muscle weakness and kidney damage or failure,

23. Synthetic Opioids
> Common names/types: Fentanyl, Actiq, Duragesic, Meperidine, Methadone
> Common uses: Pain relief
> Deadly when: Taken in excess, combined with cocaine and other drugs
> Risks: Accidental overdose

24. TMP/SMX
> Common names/types: Bactrim, Sulfatrim
> Common uses: Antibiotic
> Deadly when: Combined with antihypertensive agents
> Risks: Hyperkalemia
[in-text-ad-2]

25. Tobacco
> Common names/types: Cigarettes, cigars, pipe tobacco, chew
> Common uses: Stimulant
> Deadly when: Used over time
> Risks: Lung disease, heart disease, cancer
Detailed Findings
All of these drugs can be fatal when misused, either by consuming too much or by consuming them in lethal mixtures. Each substance poses a different level of immediate and long-term risk based on its chemical composition as well as how it tends to be used.
For instance, alcohol and tobacco are tied to far more deaths than any other drug. Alcohol is linked to approximately 88,000 deaths per year, and smoking is linked to as many as 540,000 deaths. There were 64,000 drug overdose deaths recorded in 2016. However, with use rates considerably higher for alcohol and tobacco than for opioids, a per-user death rate would reveal a different comparison.
Every drug, even those that are frequently made and sold illicitly, are useful in certain cases. Cocaine has several medical uses to this day. MDMA, commonly known as ecstasy, is being considered for its therapeutic properties in psychiatric patients. And with alcohol and tobacco, it is overuse that leads to adverse effects and deaths (although any level of tobacco use is considered overuse). With illicit and legal opioid products, it is misuse that leads to danger to the individuals and society.
Many of the problems with misuse in illicitly produced drugs exist with legally prescribed drugs. Schnoll noted that even in the instance of a prescription drug overdose, the victim often is not the same person who was prescribed the drug. “[O]ne way or another, the drug is leaking outside of the normal system,” he said.
While the problems of controlled and illicit substances stem from very different sources, the individuals most vulnerable to either set of substances share the same stigmatization. The already high risk of adverse drug outcomes among individuals with substance use disorders is amplified in a climate where drug users are criminalized and where addiction is considered a personal failing.
To illustrate the problem, Schnoll gave the example of payment mechanisms for treatment programs for patients with diabetes and patients with a substance use disorder. In the former case, when patients do not take their insulin or start eating foods they should not eat, the insurance company pays for an intensified treatment program. By contrast, patients failing regimens in drug addiction treatment programs are cut off immediately.
One of the factors making many of these drugs the most dangerous is not conscious misuse, but a lack of information for doctors and patients alike. Some potentially deadly combinations are only now being discovered, and not all physicians are fully aware of the potential consequences. Also, doctors have little control over the over-the-counter drugs their patients take, and patients may not have all the information about the risks of combining a prescribed medication and an over-the-counter drug like Aspirin or Tylenol.
While the drug-death problem cannot be traced simply to the practice of improperly prescribing medication, nearly half of all opioid overdose deaths involve a prescription opioid. The Drug Enforcement Administration (DEA) reported in November a record during its semi-annual National Prescription Drug Take Back Day. The agency received 912,305 pounds of potentially dangerous, expired, unused prescription drugs, up significantly from the previous year’s event, bringing the total since 2010 to well over 9 million pounds.
Nationwide in 2016, more than 4 billion pharmaceutical products were filled by retail pharmacies, including new and refill prescriptions, according to the non-profit health policy organization Kaiser Family Foundation.
Methodology
To identify the 25 most dangerous drugs, 24/7 Tempo reviewed a variety of data and sources, including injury and death statistics for illicit and controlled substances from the Substance Abuse and Mental Health Services Administration (SAHMSA), deadly combinations of pharmaceutical drugs and other substances from MedScape and other sources, and deadly combinations of illicit and prescribed substances from DrugAbuse.com. These combinations are selected due to their prevalence in society and the severity of their adverse effects. Items on this list are in no particular order. Many of the drugs on this list are safe for the vast majority of users.
The American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM-5) serves as the most authoritative text on the classification of mental and substance use-related diseases. In the latest volume, the set of symptoms named substance abuse and substance dependence are now called substance use disorders.
Credit Card Companies Are Doing Something Nuts
Credit card companies are at war. The biggest issuers are handing out free rewards and benefits to win the best customers.
It’s possible to find cards paying unlimited 1.5%, 2%, and even more today. That’s free money for qualified borrowers, and the type of thing that would be crazy to pass up. Those rewards can add up to thousands of dollars every year in free money, and include other benefits as well.
We’ve assembled some of the best credit cards for users today. Don’t miss these offers because they won’t be this good forever.
Flywheel Publishing has partnered with CardRatings for our coverage of credit card products. Flywheel Publishing and CardRatings may receive a commission from card issuers.
Thank you for reading! Have some feedback for us?
Contact the 24/7 Wall St. editorial team.
 24/7 Wall St.
24/7 Wall St. 24/7 Wall St.
24/7 Wall St. 24/7 Wall St.
24/7 Wall St. 24/7 Wall St.
24/7 Wall St.


